A 19 year old male with DKA
Viharika Vupputuri
Roll no- 144
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent.
Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.
This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.
I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
CASE PRESENTATION
A 19 year old male came to the OPD on 24th March with the chief complaints of
a) Vomiting since 2 days
b) Shortness of breath on 24th of march
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic one and half ago, then he developed polyuria, nocturia, polydypsia one and half year ago, was diagnosed as Diabetic type 1 MISC post COVID and during the hospital stay, on day 5 he went to coma for 7 days, then recovered and discharged after 20 days.
About 4 months ago, he developed vomitings, which was non projectile type , food and water as content, DKA 2° to DM
Now the patient presented with vomiting 10 episodes in 2 days which subsided after the patient admitted in the hospital. Non-projectile type of vomiting associated with nausea and abdominal discomfort and had food particles as contents which is not blood stained.
History of outside food consumption.
Shortness of breath was insidious in onset.
No h/o loose stools, fever, cold, cough, abdominal pain and burning micturation.
PAST HISTORY
Not a known case of Hypertension , Asthma , Epilepsy , Tuberculosis.
PERSONAL HISTORY
Daily routine
8am - Wakes up
9am- Breakfast
10am to 1pm goes to college
2pm- Lunch
3pm to 6pm- Goes out with friends
8 pm- Dinner
9pm- Sleep
Diet - Adequate
Appetite - Normal
Bowel and bladder movements - Regular
Sleep - Adequate
Addictions - No addictions
Allergies - No allergies
FAMILY HISTORY
Insignificant.
TREATMENT HISTORY
Insulin injections
Morning - 52 units
Afternoon - 26 units
Night - 52 units
GENERAL EXAMINATION
Patient was conscious, coherent and cooperative examined in a well lit room.
Patient is moderately built and well nourished.
Weight: 75 kgs
Height: 167cms
BMI: 27.7
Pallor - Absent
Icterus - Absent
Clubbing - Absent
Cyanosis - Absent
Lymphadenopathy - Absent
Edema - Absent
VITALS
Temperature - Afebrile
Blood pressure - 120/80 mmHg
Respiratory rate - 18 cpm
Pulse rate - 76 bpm
SpO2 - 96% on RA
GRBS - 157 mg/dl
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM
Bilateral air entry present
CARDIOVASCULAR SYSTEM
S1, S2 sounds heard
Murmurs - Not heard
CENTRAL NERVOUS SYSTEM - NAD
ABDOMEN
Inspection
Shape of the abdomen - Distended
Umbilicus - transverse slit like
All quadrants are moving equally with respiration
Skin over the abdomen - Normal
Superficial veins - Not visible
Palpation
No rise in temperature
Tenderness in all quadrants - Absent
Light palpation- all quadrants are normal, no pain
Deep palpation- lipodystrophy felt on right iliac fossa
Liver - Not enlarged
Spleen - not enlarged
Kidneys - bimodal palpable kidneys
Percussion
No shifting dullness
Auscultation
Bowel sounds - heard
No bruit
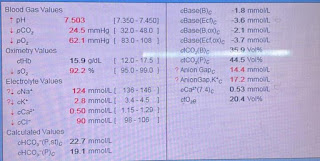
INVESTIGATIONS
SERUM ELECTROLYTE
BLOOD SUGAR
BLOOD UREA
GLYCATED HAEMOGLOBIN
LIVER FUNCTION TESTS
PHOSPHORUS
SERUM CREATININE
BLOOD SUGAR - FASTING
KETONE BODIES
ECG
USG ABDOMEN
Impression - Grade 1 Fatty liver
PROVISIONAL DIAGNOSIS
Diabetic ketoacidosis 2° to ? inadequate insulin, ?Acute Gastroenteritis.
TREATMENT
IVF - 20NS 20RL @100ml/hr
Inj.HUMAN ACTRAPID 40U in 39ml NS @ 5ml/hr
Inj.PANTOP 40 mg IV / OD
Inj.ZOFER 4 mg IV / TID
Inj.NEOMOL 1g IV / SOS
Tab.DOLO 650 mg PO / TID
Inj. 5%dextrose 50ml/hr
Inj.MONOCEF 1gm IV / BD
Strict GRBS , BP Charting
.png)




.png)













Comments
Post a Comment