36 year old male with angioedema
36 year old male with angioedema
Viharika Vupputuri
Roll no- 144
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent.
Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.
This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.
I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
CASE PRESENTATION
A 36 yr old male patient who is a watchman in a government hospital was admitted at 4AM on 12/01/2022 in the OPD with the chief complaints of
1) Discomfort of the throat since 3-4 hrs
2) Swelling and pain in the throat
HISTORY OF PRESENTING ILLNESS
Patient was working asusual and then he developed swelling in the throat at 1AM in the morning of 12/01/2022.
Then he went to check himself in the mirror to examine and noticed swelling of throat.
Patient noticed that the swelling started at uvula and progressed down till the whole throat is involved.
The swelling presented by the patient is sudden in onset and gradually progressive in nature since morning.
Pain is sudden in onset and gradually progressive in nature.
Patient was not able to turn his neck side to side.
PAST HISTORY
Patient had similar complaints in the past.
He was apparently asymptomatic 15 years back then he developed first episode of swelling in the throat associated with pain so he went to a local hospital and was referred to our hospital where tracheostomy was done.
He also had history of multiple swellings over the body which persists for atleast 3 days after using hydrocortisone.
It is not associated with redness, itching and irritation.
Swelling occurred in specific site would rapidly progress throughout the body.
This occurs atleast 2 times a month which is intermittent and random.
Swelling would occur on the face, trunk, upper and lower limb. Common site is face and limbs.
Then he developed 2nd episode in 2016 with complaints of swelling of base of tongue and uvula and tracheostomy was done.
He was not able to regularly work due to these symptoms.
Patient is not a known case of diabetes, hypertension, asthma, epilepsy, tuberculosis.
ALLERGIC HISTORY
Food allergy - Fish, Meat(mutton), leafy vegetable (gongura), brinjal.
Smell - perfume, garbage, sanitizer and smoke.
Pollutants.
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Bowel and bladder - Regular
Sleep - Inadequate
No Addictions
FAMILY HISTORY
Not significant.
TREATMENT HISTORY
Takes avil and hydrocortisone injections whenever swelling occurs.
SURGICAL HISTORY
Undergone tracheostomy 2 times.
GENERAL EXAMINATION
Patient is conscious, coherent and cooperative and is well oriented to time, place and person.
He is well nourished and moderately built.
Pallor - Absent
Icterus - Absent
Clubbing - Absent
Cyanosis - Absent
Lymphadenopathy - Absent
Edema - Absent
VITALS
Pulse rate - 120bpm
Respiratory rate - 16cpm
BP - 120/91 mmHg
Temperature - Afebrile
SYSTEMIC EXAMINATION
EXAMINATION OF NOSE AND ORAL CAVITY
No Trismus.
Examination of oral cavity - lips, teeth,buccal mucosa and gums.
Anterior 2/3rd of tongue, hard palate and floor of the mouth appears normal.
Examination of oral pharynx - congestion and oedema of anterior pillar, uvula and soft palate. Posterior pharyngeal wall appears congested.
Examination of nose - turbinates and mucosa appears normal
RESPIRATORY SYSTEM
Examination of trachea - normal neck movements and tracheostomy scar seen.
Inspection
Shape of the chest - Bilaterally symmetrical.
Position of trachea - deviated to left side.
Crowding of ribs - Absent.
Expansion of chest - equal on both sides.
No visible pulsations.
Palpation
No tenderness
No local rise of temperature.
Bilateral air entry.
Apex beat - Heard.
Percussion - resonant in all areas
Auscultation - normal vesicular breath sound
CVS
S1,S2 are heard.
No murmurs heard
ABDOMEN
Scaphoid shaped abdomen
No tenderness and palpable mass
No free fluid
Auscultation - bowel sounds heard
Liver - Not palpable
Spleen - Not palpable
CNS EXAMINATION
Conscious
Normal speech
Cervical nerves - intact
Normal sensory and motor system
Neck stiffness - absent
Reflexes - normal
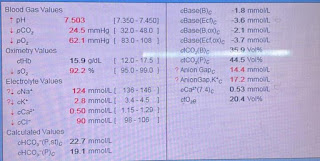
INVESTIGATIONS
PROVISIONAL DIAGNOSIS
Hereditary angioneurotic edema.
TREATMENT
1) Inj. hydrocortisone
2) Nebulization with adrenaline
3) Inj. avil i.v
4) Check BP, PR, RR, SPO2 - 2nd hrly.














Comments
Post a Comment