MEDICINE ASSIGNMENT
31st May 2021
Medicine assignment for the month of May 2021
Viharika Vupputuri
Roll no - 144
I have been given the following cases to solve in an attempt to understand
the topic of 'Patient clinical data analysis' to develop my competency
in reading and comprehending clinical data including history, clinical
findings, investigations and diagnosis and coem up with a treatment
plan.
This is the link of questions asked regarding the cases:
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
FIRST CASE :
PULMONOLOGY
A 55 year old female with shortness of breath, pedal edema and facial puffiness.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the problem and what is the primary etiology of patient's problem?
ANS - Symptoms include
- Shortness of breath - from past 20 years.
First episode of SOB which was 20 years ago lasted for 1 week and it was relieved upon taking medications.
Patient suffered from similar episodes of SOB next 8 years each lasting for 1 week and relieved upon taking medications.
She had an other episode of SOB 12 years ago which lasted for 20 days and she had to be hospitalized. SOB relieved by treatment at the hospital.
Her latest episode lasted for 30 days which was insidious in onset and gradually progressive.
Anemia and iron injections - 5 yrs ago.
- Pedal edema - since 15 days.
- Facial puffiness - since 15 days.
- Hypertension - 20 days back.
Anatomical localization of the problem -
Lungs - bronchi and bronchioles.
This led to increased blood pressure in pulmonary artery resulted in RIGHT HEART FAILURE.
Etiology - Working in paddy fields lead to inhalation of paddy dust.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ans -
Non-Pharmacological Interventions:-
1.Head end Elevation:
It increases global and regional end-expiratory lung volume. It also improves oxygenation and hemodynamic performance.
2.BiPAP Intermittent
The machine is able to provide relief to
your overworked lungs and chest wall muscles.
3.Chest physiotherapy
It
is designed to improve
respiratory efficiency, promote expansion of the lungs, strengthen
respiratory muscles, and eliminate secretions from the respiratory
system.
4.Vitals Charting:
This
allow for continuous monitoring of a patient.
5. I/O chart
Urine input/output chart
It is also known as a frequency-volume chart or bladder diary and is used
to assess how much fluid you drink, to measure your urine volume, to
record how often you pass urine over 24 hours and to show any episodes
of leakage.
6. O2 Inhalation
It is used to
- manage the condition of hypoxia
- maintain o2 tension in blood plasma
- increase oxy haemoglobin in RBC
- maintain ability of cells to carry out normal metabolic function
- reduce the risk of complications
Pharmacological Interventions -
3) What could be the causes for her current acute exacerbation?
Ans - It could be due to infection or environment pollutants.
4) Could the ATT have affected her symptoms? If so how?
Ans - ATT affects her symptoms.
Rifampicin and Isoniazid - It is nephrotoxic which rises Renal function tests.
5) What could be the causes for her electrolyte imbalance?
Ans -
Hyponatremia:
- Worsening of Hypoxia
- Respiratory acidosis
- Right heart failure
Hypochloremia:
- Respiratory acidosis with metabolic alkalosis.
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
Ans -
- 2009 (12 years ago): Started drinking alcohol
- 2019 (2 years ago): Diagnosed with Diabetes Mellitus, prescribed oral hypoglycemics
- 2020 (1 year ago): Has an episode of seizures (most likely GTCS)
- January 2021 (4months ago): Has another seizure episode (most likely
GTCS)- following cessation of alcohol for 24 hours. Starts drinking
again after seizure subsides
- Monday, May 10, 2021: Last alcohol intake, around 1 bottle. Starts having general body pains at night.
- Tuesday, May 11, 2021: Decreased food intake. Starts talking and
laughing to himself. Unable to lift himself off the bed, help required.
-Conscious,
but non coherent. Disoriented to time, person, place.Goes to an RMP the
same day- is prescribed IV fluids and asked to visit a hospital
- Saturday, May 15, 2021: Is admitted to a tertiary care hospital for
alcohol withdrawal symptoms, and is treated for the same.
Anatomical localization of the problem
The most probable location in the brain is the hippocampus and frontal lobe.

Primary etiology of the patient's problem
Chronic Alcoholism
2) What are
mechanism of action, indication and efficacy over placebo of each of the
pharmacological and non pharmacological interventions used for this
patient?
Ans -
Thiamine
Mechanism of action - Combines with adenosine triphosphate (ATP) in the liver, kidneys, and leukocytes to produce thiamine diphosphate. Thiamine diphosphate acts as a coenzyme in carbohydrate metabolism, in transketolation reactions, and in the utilization of hexose in the hexose-monophosphate shunt.
Indications - Thiamine deficiency
Neuritis
deceased appetite
Ulcerative colitis
Efficacy - thiamine reduces the risk of dementia in chronic alcoholics.
Lorazepam
MOA - Binds to benzodiazepine receptors on the postsynaptic GABA-A ligand-gated chloride channel neuron at several sites within the central nervous system.it enhances the inhibitory effects of GABA, which increases the conductance of chloride ions into the cell.
Indications - Active seizures
severe anxiety
sedation
Efficacy - It is used to treat all types of seizures.
Pregabalin
It subtly reduces the synaptic release of several neurotransmitters, apparently by binding to alpha2-delta subunits, and possibly accounting for its actions invivo to reduce neuronal excitability and seizures.
Lactulose
It is used in preventing and treating clinical portal-systemic encephalopathy .its chief mechanism of action is by decreasing the intestinal production and absorption of ammonia.
Potchlor liquid
It is used to treat low levels of potassium in the body.
3) Why have neurological symptoms appeared this time, that where absent during withdrawal earlier? What could be a possible cause for this?
4) What is the reason for giving thiamine in this patient?
Ans -
Differential diagnosis for altered sensorium following chronic
alcoholism is Wernicke-Korsakoff Syndrome, caused by deficiency of
thiamine (B1). To treat thiamine
is given.
Thiamine is necessary to provide energy to the CNS, helps in conduction of nerve signals.
Deficiency leads to confusion and ataxia.
5) What is the probable reason for kidney injury in this patient?
Ans -
As the urea levels are very high, it leads to Acute Renal Failure.
As
high serum creatinine, and urea levels are present, shows that
reabsorption from tubules is taking place .Therefore the primary cause
is prerenal, most probably due to generalised dehydration.
A
slightly high FENa level also denotes that tubular necrosis . Hence the Prerenal AKI leading to Acute Tubular Necrosis (ATN).
6) What is the probable cause for the normocytic anemia?
Ans -
- Alcohol causes iron deficiency by causing defect in cell production.
- Decreased bone marrow production of RBCs, due to EPO deficiency owing to kidney failure
- Loss of blood through chronic foot ulcer
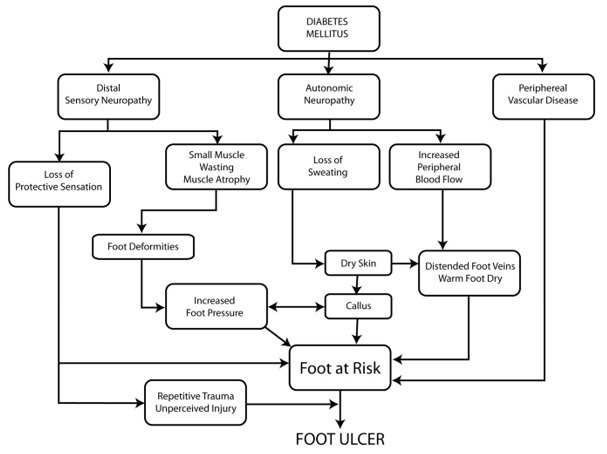
7) Could chronic alcoholism have aggravated the foot ulcer formation?
Ans -
Yes,
as alcoholism can cause peripheral neuropathy which along with Diabetic neuropathy leads to a
non-healing foot ulcer.
B) A 52 year old male with cerebellar ataxia.
1) What is the evolution of the
symptomatology in this patient in terms of an event timeline and where
is the anatomical localization for the problem and what is the primary
etiology of the patient's problem?
Ans -
7 days back- Patient gave a history of giddiness that started around 7 in the morning; subsided upon taking rest; associated with one episode of vomiting
4 days back- Patient consumed alcohol; He developed giddiness
H/O postural instability- falls while walking
Associated with bilateral hearing loss, aural fullness, presence of tinnitus
Associated vomiting- 2-3 episodes per day
Present day of admission- Slurring of speech, deviation of mouth that got resolved the same day
Anatomical location - There is a presence of an infarct in the inferior cerebellar hemisphere of the brain.
Etiology - Ataxia is the lack of muscle control or co-ordination of voluntary movements, such as walking or picking up objects. This is usually a result of damage to the cerebellum
Conditions cause cerebellar ataxia- Head trauma, Alcohol abuse, certain medications eg. Barbituates, stroke, tumours, cerebral palsy, brain degeneration etc.
The patient has hypertension for which he has been prescribed medication that he has not taken. Stroke due to an infarct can be caused by blockade or bleeding in the brain due to which blood supply to the brain is decreased, depriving it of essential oxygen and nutrients. This process could’ve caused the infarct formation in the cerebellar region of the brain, thus causing cerebellar ataxia.
2) What are
mechanism of action, indication and efficacy over placebo of each of the
pharmacological and non pharmacological interventions used for this
patient?
Ans -
A) Tab Vertin 8mg- This is betahistine, which is an anti- vertigo medication
MOA- It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability. This can reverse the underlying problem.
Indications- Prescribed for balance disorders. In this case it is used due to patients history of giddiness and balance issues.
B) Tab Zofer 4mg- This is ondanseteron- It is an anti emetic
MOA- It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
Indications- Used to control the episodes of vomiting and nausea in this patient.
C) Tab Ecosprin 75mg- This is aspirin. It is an NSAID
MOA- They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis
Indications- They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
D) Tab Atorvostatin 40mg- This is a statin
MOA- It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases
Indications- Used to treat primary hyperlipidemias. In this case it is used for primary prevention of stroke.
E) Clopidogrel 75mg- It is an antiplatelet medication
MOA- It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
Indications- In this case it decreases the risk of heart disease and stroke by preventing clotting
F) Thiamine- It is vitamin B1
It is naturally found in many foods in the human diet. In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
Indications- Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
G) Tab MVT- This is methylcobalamin
Mainly given in this case for vitamin B12 deficiency.
3) Did the patients history of denovo HTN contribute to his current condition?
Ans -
A cerebellar infarct is usually caused by a blood clot obstructing blood flow to the cerebellum. High blood pressure that is seen in hypertension (especially if left untreated) can be a major risk factor for the formation of cerebellar infarcts.
Increased shear stress is caused on the blood vessels. The usual adaptive responses are impaired in this case, thus leading to endothelial dysfunction in this case. High BP can also promote cerebral small vessel disease. All these factors contribute to eventually lead to stroke.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
Ans -
Meta analysis of the relation between alcohol consumption and increased risk of stroke has mainly weighed in to the formation of two types- ischaemic and haemorrhagic stroke.
Ischaemic stroke- this is more common. This Is caused by a blood clot blocking the flow of blood and preventing oxygen from reaching the brain
Haemorrhagic stroke- occurs when an aneurysm bursts or when a weakened blood vessel leaks, thus causing cerebral haemorrhage
C) A 45 year old female patient with palpitations, pedal edema, chest pain, chest heaviness, radiating pain along left upper limb.
1) What is the evolution of the
symptomatology in this patient in terms of an event timeline and where
is the anatomical localization for the problem and what is the primary
etiology of the patient's problem?
Ans -
Evolution of symptoms -
- Patient was normal 8 months back then developed b/l pedal edema which gradually progressed.
Aggerevated in sitting and standing position, relived on taking medication
- Palpitations - Since 5days, sudden in onset which is more during night
Aggerevated by lifting heavy weights, speaking continuously
- Dyspnoea - Since 5 days
- Pain - Since 6days, radiating along left upper limb, more during palpitations and relived on medication.
- Chest pain associated with chest heaviness since 5 days
Anatomical localisation -Palpitations.
Etiological agent
- Electrolyte imbalance (hypokalemia) causes manifestations like palpitations, chest heaviness, generalised body
weakness.
- Radiating pain along her left upper limb due to cervical spondylosis
2) What are the reasons for recurrence of hypokalemia in her? Important risk
factors for her hypokalemia?
Ans -
Recurrent hypokalemic periodic paralysis
Current risk factor - Use of diuretics
Other risk factors
A) Abnormal loses
Medications-diuretics, laxatives, enema, corticosteriods
Real causes- osmotic diuresis, mineralo corticoid excess, renal tubular acidosis, hypomagnesenemia
B) Trance cellular shift - alkalosis, thyrotoxicosis, delirium tremans, head injury, Myocardial, ischemia, recurrent hypokalemic periodic paralysis
C) Inadequate intake - anorexia, dementia, stareation, total parental nutrition
D) psuedohypokalemia - delayed sample analysis, significant leukocytosis
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
Ans -
Changes seen in ECG -
Earliest
change - decreased T-wave amplitude, ST depression, Twave - and
inversion or flat;prolonged PR interval;presence of Uwaves
In Severe cases - ventricular fibrillation, rarely AV block
Symptoms of hypokalemia-
Weakness & fatigue, palpitations, muscle cramps & pain, anxiety, psychosis, depression, delirium.
D) 55 year old patient with seizures.
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
Ans -
Occurrence of seizure due to brain stroke
Cells
in the brain send electrical signals to one another. The electrical
signals pass along your nerves to all parts of the body. A sudden
abnormal burst of electrical activity in the brain can lead to the
signals to the nerves being disrupted, causing a seizure. This
electrical disturbance can happen because of stroke damage in the brain.
A
seizure can affect you in many different ways such as changes to
vision, smell and taste, loss of consciousness and jerking movements.
Mechanism of seizure activity
You’re
more likely to have a seizure if you had a haemorrhagic stroke . Seizures can also be more likely if you had a severe
stroke .
Some people will have repeated seizures, and be
diagnosed with epilepsy. The chances of this happening may depend on
where the stroke happens in the brain and the size of the stroke.
2.
In the previous episodes of seizures, patient didn't loose his
consciousness but in the recent episode he lost his consciousness what
might be the reason?
Ans -
Consciousness system - It is a specialized set of
cortical-subcortical structure which maintains alertness, attention and
awareness.
Diverse seizure types including absence, generalized
tonic-clonic and complex partial seizures converge on the same set of
anatomical structures through different mechanisms to disrupt
consciousness.
E) A 48 year old male with seizures and altered sensorium.
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
Ans - CT scan showed that the patient has cerebral haemorrhage in frontal lobe caused due to minor head injuries which leads to Frontal lobe ataxia.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses?
Ans -
After minor head injuries the haemorrhages should be cured on itself if present. As the patient is a chronic alcoholic this might have stopped the process of healing or it may increase the size of haemorrhage .
F) A 30 year old male patient with weakness of right upper limb and lower limb.
1) Does the patient's history of road traffic accident have any role in his present condition?
Ans - There is a role of road traffic accident in his present condition which was unidentified. The closeness of facial bones to the cranium would suggest that there are chances of cranial injuries. Since the Zygomatic arch and Mandibular process is very close to the cranium, this might play a role in the patient's present condition
2) What are the warning signs of CVA?
Ans - a) Sudden loss of eye sight in one or both the eyes.
b) Sudden trouble in walking, speaking and understanding speech.
c) Sudden weakness or numbness in arms, legs and face especially on one side.
d) Sudden dizziness, loss of balance and confusion.
e) Sudden headache without any known cause.
3) What is the drug rationale in CVA?
Ans -
Mannitol- Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
Ecospirin
Atrovas-Atorva 40 Tablet belongs to a group of medicines called statins. It is used to lower cholesterol and to reduce the risk of heart diseases. Cholesterol is a fatty substance that builds up in your blood vessels and causes narrowing, which may lead to a heart attack or stroke.
4) Does alcohol has any role in his attack?
Ans -
When the patient met with an accident there might be cranial damage which was unnoticed.
If so his occasional drinking may or may not have hindered the process of the minor hemorrhages getting healed and might have caused this condition
But since the patient is not a chronic alcoholic and so Alcohol might not have played any role.
5) Does his lipid profile has any role for his attack?
Ans - Lipid profile doesn't show have any role in this attack.
G) A 50 year old patient with cervical myelopathy.
1) What is myelopathy hand?
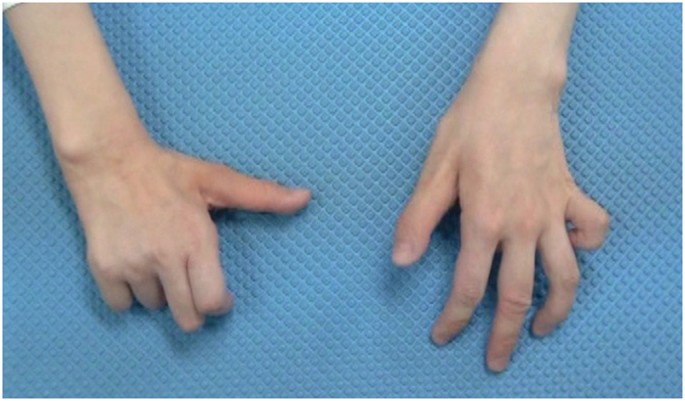
Ans - Loss of power of extension and adduction in the ulnar 2 or 3 fingers and inability to grip and release rapidly is known as Myelopathy hand.
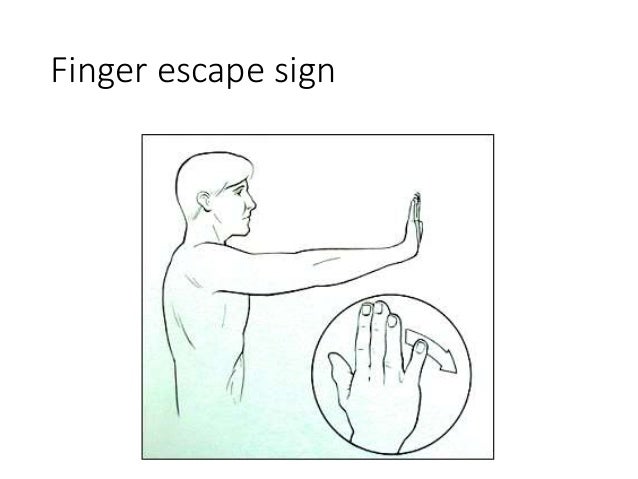
2) What is finger escape?
Ans - It is a neurological sign. Called as Wartenberg's sign.
It is involuntary abduction of 5th finger caused by unopposed action of extensor digiti minimi.
3)What is Hoffman's reflex?
Ans - It is a test to examine the reflexes of upper extremities.
This test is to test for existence of spinal cord compression or any underlying nerve condition.
H) 17 year old female with seizures.
1)What can be the cause of her condition?
Ans - Cortical vein thrombosis might be the cause of her seizures.
2) What are he risk factors for cortical vein thrombosis ?
Ans - Risk factors are:
Blood clots
Sickle cell anemia
Iron deficiency
Chronic hemolytic anemia
Heart disease
Dehydration.
3) There was seizure free period in between but again sudden episode of
GTCS why? resolved spontaneously why?
Ans -
Seizures are resolved and seizure free period got achieved after medical intervention but sudden episode of seizure was may be due to any persistence of excitable foci by abnormal firing of neurons.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
Ans - Injection Clexane 0.4ml given subcutaneously twice a day.
THIRD CASE
CARDIOLOGY
A) A 78 year old male with shortness of breath, chest pain, bilateral pedal edema and facial puffiness.
1.What is the difference between heart failure with preserved ejection fraction and with reduced ejection fraction?
Ans -
Preserved ejection fraction – referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Reduced ejection fraction – referred to as systolic heart failure
2.Why haven't we done pericardiocenetis in this patient?
Ans - As the effusion was self healing, pericardiocentesis.
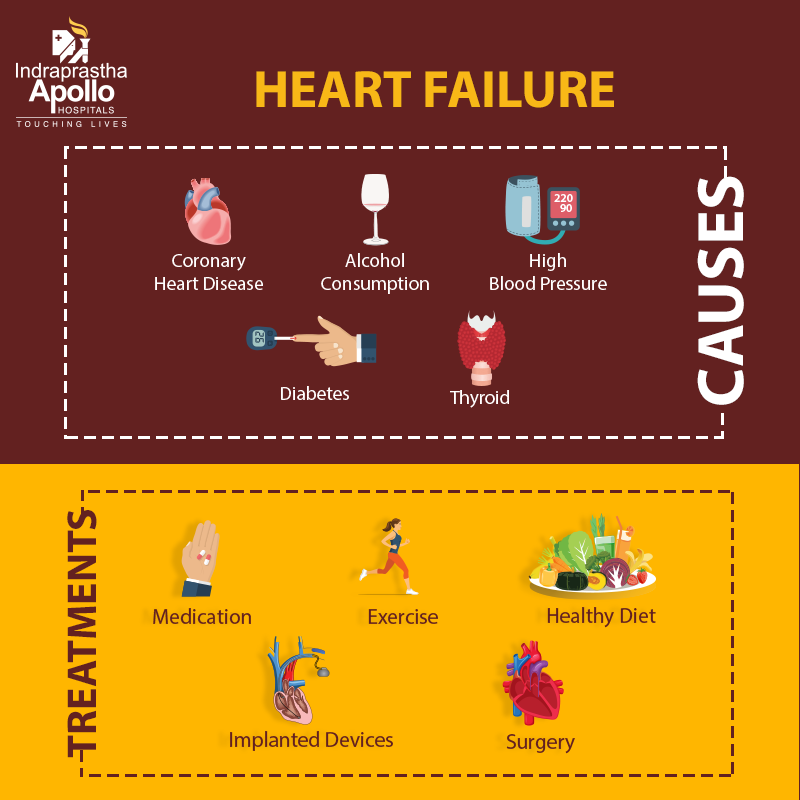
3.What are the risk factors for development of heart failure in the patient?
Ans -
-Alcohol abuse
- High BP
- Smoking
- Diabetes
- AV block can be associated with severe bradycardia and hemodynamic instability
4.What could be the cause for hypotension in this patient?
Ans - Thickening of visceral pericardium may restrict heart to expand which causes hypotension.
B) A 73 year old male patient with pedal edema, shortness of breath and decreased urine output.
1.What are the possible causes for heart failure in this patient?
Ans - Major causes of heart failure -
1) 30 years ago patient diagnosed with type 2 DM
- Patient also diagnosed with diabetic triopahy indicating uncontrolled diabetes.
2) Hypertension - 19 years ago.
3) Chronic alcoholic - 40 years ago
4) Elevated creatinine and AST/ASL ratio >2 and with chronic kidney disease IV
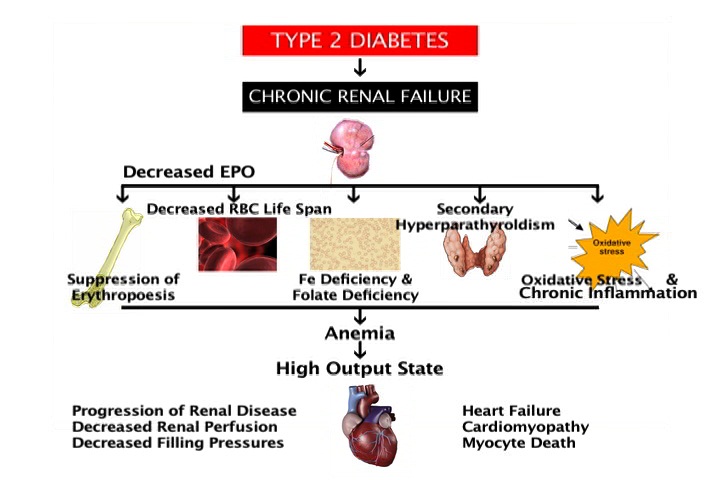
2. What is the reason for anemia in this case?
Ans -
Chronic kidney disease results in decreased production of erythropoietin which in turn decreases the production of red blood cells from the bone marrow.
Patient’s with anaemia and CKD also tend to have deficiency in nutrients like iron, vitamin B12 and folic acid essential in making healthy red blood cells
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
Ans - Reason for blebs and non healing ulcer is DIABETES MELLITUS
Delay in healing of wounds along with poorly controlled diabetes caused by CKD.
Anaemia can also slow down the process of healing due to low oxygen levels.
4. What sequence of stages of diabetes has been noted in this patient?
Ans - There are 4 stages in type 2 diabetes--Insulin resistance
-Prediabetes
-Type 2 diabetes
-Vascular complications, including retinopathy, nephropathy or neuropathy and related microvascular events.
C) A 52 year old male patient with A-Fib and bilateral thrombus.
1) What is the evolution of the
symptomatology in this patient in terms of an event timeline and where
is the anatomical localization for the problem and what is the primary
etiology of the patient's problem?
Ans -
Evolution of symptomatology -
Shortness of breath - 2 days ago
Decreased urine output - 2 days ago
Anuria - since morning
The anatomical site is BLOOD VESSELS
ETIOLOGY -
The physical stress of hypertension on the arterial wall also results in the aggravation and acceleration of atherosclerosis, of the coronary and cerebral vessels. Hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
The cause of arterial thrombosis is artery damage due to atherosclerosis.
2)
What are mechanism of action, indication and efficacy over placebo of
each of the pharmacological and non pharmacological interventions used
for this patient?
Ans -
PHARMACOLOGICAL INTERVENTIONS
1. TAB. Dytor
Mechanism - Its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB. Acitrom
Mechanism - Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. Cardivas
Mechanism - Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI
Mechanism - Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.TAB. Digoxin
Mechanism -
Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
a) Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump,
b) An enzyme that controls the movement of ions into the heart.
6. Hypoglycemia symptoms
7. Bleeding manifestations - Petechiae, Bleeding gums.
8. APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
3)
What is the pathogenesis of renal involvement due to heart failure
(cardio renal syndrome)? Which type of cardio renal syndrome is this
patient?
Ans - cardiorenal syndrome type 4 is seen in this patient.
4) What are the risk factors for atherosclerosis in this patient?
Ans -
They impair ability of blood vessels to relax and stimulate the growth of smooth muscle cells inside arteries. All these changes can contribute to the artery-clogging process known as atherosclerosis.
5) Why was the patient asked to get those APTT, INR tests for review?
Ans -
APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
D) 67 year old patient with acute coronary syndrome
1) What is the evolution
of the symptomatology in this patient in terms of an event timeline and
where is the anatomical localization for the problem and what is the
primary etiology of the patient's problem?
Ans -
Evolution of sympomaology
-Diabetes since 12 years - on medication
-Heart burn like episodes since an year- relieved without medication
-Diagnosed with pulmonary TB 7 months ago- completed full course of treatment, presently sputum negative.
-Hypertension since 6 months - on medication
-Shortness of breath since half an hour-SOB even at rest
Anatomical localisation - Cardiovascular system
Etiology - The patient is both Hypertensive and diabetic , both these conditions can cause
Atherosclerosis - there is build up of fatty and fibrous material inside the wall of arteries.(PLAQUE)
2)
What are mechanism of action, indication and efficacy over placebo of
each of the pharmacological and non pharmacological interventions used
for this patient?
Pharmacological interventions
TAB MET XL 25 MG/STAT-contains Metoprolol as active ingredient
MOA - METOPROLOL is a cardiselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect) and with less force( negative inotropic effect).
Beta blockers also help open up your veins and arteries to improve blood flow.
Indications - it is used to treat Angina, High blood pressure and to lower the risk of hear attacks .
Non pharmacological intervention
PERCUTANEOUS CORONARY INTERVENTION.
It is a non-surgical procedure that uses a catheter (a thin flexible tube) to place a small structure called a stent to open up blood vessels in the heart that have been narrowed by plaque buildup ( atherosclerosis).
3) What are the indications and contraindications for PCI?
Ans -
INDICATIONS:
- Acute ST-elevation myocardial infarction (STEMI)
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Unstable angina.
- Stable angina.
- Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
CONTRAINDICATIONS:
-Intolerance for oral antiplatelets long-term.
-Absence of cardiac surgery backup.
-Hypercoagulable state.
-High-grade chronic kidney disease.
-Chronic total occlusion of SVG.
-Artery with a diameter of <1.5 mm.
4)
What happens if a PCI is performed in a patient who does not need it?
What are the harms of overtreatment and why is research on overtesting
and overtreatment important to current healthcare systems?
Ans -
PCI is generally a safe procedure , it might cause serious certain complications like
A)Bleeding
B) Blood vessel damage
C) Allergic reaction to the contrast dye used
D) Arrhythmias
E) Need for emergency coronary artery bypass grafting .
All these complications it is better to avoid PCI in patients who do not require it.
E) A 60year old Male patient with chest pain, giddiness and sweating.
1) What is the evolution
of the symptomatology in this patient in terms of an event timeline and
where is the anatomical localization for the problem and what is the
primary etiology of the patient's problem?
Ans -
Anatomical location of etiology is BLOOD VESSELS.
Myocardial infarction is usually due to thrombotic occlusion of a coronary vessel caused by rupture of a vulnerable plaque. Ischemia induces profound metabolic and ionic perturbations in the affected myocardium and causes rapid depression of systolic function
2)
What are mechanism of action, indication and efficacy over placebo of
each of the pharmacological and non pharmacological interventions used
for this patient?
Ans -
PHARMACOLOGICAL INTERVENTION
1.TAB. ASPIRIN
Mechanism - Aspirin inhibits platelet function through irreversible inhibition of cyclooxygenase (COX) activity. Until recently, aspirin has been mainly used for primary and secondary prevention of arterial antithrombotic events.
2.TAB ATORVAS
Mechanism - Atorvastatin competitively inhibits 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. By preventing the conversion of HMG-CoA to mevalonate, statin medications decrease cholesterol production in the liver.
3.TAB CLOPIBB
Mechanism - The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP- mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible.
4.INJ HAI
Mechanism - Regulates glucose metabolism
Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue
5.ANGIOPLASTY
Mechanism - Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
Ans -
Second PCI was NOT necessary in this patient.
PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.
F) An 87 year old male with shortness of breath, constipation and decreased urine output.
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
Ans -
The fluid loss occurred to the patient
there is decreased preload- so, SOB occurred due to decreased CO
IV fluids administered- there is increased preload- SOB decreased due to better of cardiac output.
2. What is the rationale of using torsemide in this patient?
Ans - Torsemide used to relieve abdominal distension.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Ans -
IT IS THE TREATMENT FOR UTI
Rationale- Used for any bacterial infection.
4) Gastroenterology
A) A 33year old male with pancreatitis, psuedocys and lef broncho pleural fistula.
1)
What is the evolution of the symptomatology in this patient in terms of
an event timeline and where is the anatomical localization for the
problem and what is the primary etiology of the patient's problem?
Ans -
Evolution of symptomatology
5 years back-1st episode of pain abdomen and vomitings
Stopped taking alcohol for 3 years
1 year back 5 to 6 episodes of pain abdomen and vomitings after starting to drink alcohol again
20 days back increased consumption of toddy intake
Since 1 week pain abdomen and vomiting
Since 4 days fever constipation and burning micturition
Anatomical localisation - Pancreas and left lung
Alcohol and its metabolites produce changes in the acinar cells, which may promote premature intracellular digestive enzyme activation thereby predisposing the gland to autodigestive injury. Pancreatic stellate cells (PSCs) are activated directly by alcohol and its metabolites and also by cytokines and growth factors released during alcohol-induced pancreatic necroinflammation. Activated PSCs are the key cells responsible for producing the fibrosis of alcoholic chronic pancreatitis
2)
What is the efficacy of drugs used along with other non pharmacological
treatment modalities and how would you approach this patient as a
treating physician?
Ans -
Non pharmacological interventions : drains ( malecot & icd )
Even i as a treating physician will follow the same approach
B) A 25 year old male with epigastric pain.
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
Ans - PLEURAL EFFUSION is he cause of dyspnea.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
Ans -
This hyperglycemia could thus be the result of a hyperglucagonemia secondary to stress
The result of decreased synthesis and release of insulin secondary to the damage of pancreatic β-cells
Elevated levels of catecholamines and cortisol
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
Ans -
LFT are increased due to hepatocyte injury
- If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage.
- Elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
4) What is the line of treatment in this patient?
Ans -
Plan of action and Treatment:
Investigations:
✓ 24 hour urinary protein
✓ Fasting and Post prandial Blood glucose
✓ HbA1c
✓ USG guided pleural tapping
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
C) A 45 year old Female patient with Fever, Pain abdomen, Decreased Urine output and Abdominal distension.
1) what is the most probable diagnosis in this patient?
Ans - Liver abscess
Hollow viscous perforation
Intraperitoneal hematoma
Grade 3 RPD of right kidney.
Most probable diagnosis - Abdominal hemorrhage
·
· 2) What was the cause of her death?
Ans - Paient went to hyderabad after leaving the hospital and underwent laparotomy surgery. The patient passed away next day.
Causes of death - hemorrhage and infecion
3) Does her NSAID abuse have something to do with her condition? How?
NSAID-induced
renal dysfunction has a wide spectrum of negative effects, including decreased
glomerular perfusion, decreased glomerular filtration rate, and acute renal
failure.
Adverse effects - gastrointestinal mucosa injury.
5) Nephrology
A) A52 year old male patient with shortness of breath, burning micturation and fever.
1. What could be the reason for his SOB ?
Ans - Acidosis caused by diuretics is the reason for SOB
2. Why does he have intermittent episodes of drowsiness ?
Ans - Hyponatremia was the cause for his drowsiness
3. Why did he complaint of fleshy mass like passage in his urine?
Ans - Plenty of pus cells in his urine passage appeared as fleshy mass like passage to him.
4. What are the complications of TURP that he may have had?
Ans - Difficulty micturition
Electrolyte imbalances
Infection
B) A 8 year old boy with frequent urination.
1.Why is the child excessively hyperactive without much of social etiquettes ?
Ans -
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity.
For a diagnosis, the symptoms have to be present for more than six months.
2. Why doesn't the child have the excessive urge of urination at night time ?
Ans -
1. Psychosomatic disorder
2. Undiagnosed anxiety disorder
3. How would you want to manage the patient to relieve him of his symptoms?
- Bacterial kidney infection - the typical course of treatment is antibiotic and painkiller therapy.
If the cause is an overactive bladder, a medication known as an anticholinergic may be used. These prevent abnormal involuntary detrusor muscle contractions from occurring in the wall of the bladder
To treat attention deficit hyperactivity disorder:
For children 6 years of age and older, the recommendations include medication and behavior therapy together — parent training in behavior management for children up to age 12 and other types of behavior therapy and training for adolescents. Schools can be part of the treatment as well.
Methylphenidate A stimulant and a medication used to treat Attention Deficit Hyperactivity Disorder. It can make you feel very ‘up’, awake, excited, alert and energised, but they can also make you feel agitated and aggressive. They may also stop you from feeling hungry.
Amphetamine belongs to a class of drugs known as stimulants. It can help increase your ability to pay attention, stay focused on an activity, and control behavior problems. It may also help you to organize your tasks and improve listening skills.
6) Infectious Disease
A 40 year old female with dysphagia, fever and cough.
1)Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
Ans - Cough - since 2 months on taking food and liquids
- Difficulty in swallowing since 2 month . It was initially difficult only with solids but then followed by liquids also.
- Laryngeal crepitus- positive
These favour for tracheo esophageal fistula
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
Ans -
Immune reconstitution inflammatory syndrome (IRIS) represents the worsening of a recognized (paradoxical IRIS) or unrecognized (unmasking IRIS) pre-existing infection in the setting of improved immunologic function.
The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
7) Infectious disease and Hepatology
A) A 55 year old male patient with pain abdomen,decreased appetite and fever.
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?
Ans - Yes, it could be due to intake of contaminated toddy
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
Ans - Alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver. It is also proven that Alcoholism is never an etiological factor for the formation of liver abscess.
3. Is liver abscess more common in right lobe ?
Ans - Right lobe is involved due to its moreblood supply
4.What are the indications for ultrasound guided aspiration of liver abscess ?
Ans -
1. Large abscess more than 6cms
2. Left lobe abscess
3.Caudate lobe abscess
4. Abscess which is not responding to drugs
B) A 21 year male student with abdominal pain and fever.
1) Cause of liver abcess in this patient ?
Ans -
The patient is occasional toddy drinker which has high amount of Entamoeba histolytica. This causes liver abscess by suppressing the function of Kuffper cells.Therefore Toddy is most probable cause of Liver abscess in this patient
2) How do you approach this patient ?
Ans -
Hematology -
- Common hematological finding being LEUCOCYTOSIS , indicating inflammation or infection.
-Anemia may be present , or not.
Chemistry-
-Elevated liver enzymes such as AST,ALP are noted .
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
Ans -
- INJECTION ZOSTUM 1.5 gm IV BD (twice daily)
Zostum is a combination of drugs - SULBACTUM (pencillin) & CEFOPERAZONE(cephalosporin) [Antibiotic]: It is used here to treat if any bacterial cause ( since we can’t take the risk relying on only anti amoebic therapy)
- INJECTION. METROGYL 500mg IV TID ( thrice daily )
Metrogyl has the drug called METRONIDAZOLE[Antibiotic]: For amoebic cause
- INJECTION. OPTINEURIN 1amp in 100 ml NS( Normal Saline) IV OD ( once daily)
Optineurin is a multivitamin drug { A combination of B1,B2, B3, B5,B6, B12 } given here as a supplement
- TAB. ULTRACET 1/2 QID( four times a day)
Ultracet is a combination of drugs - TRAMADOL(opiod analgesic) and ACETAMINOPHEN (analgesic and antipyretic) : Given for pain and fever
- TAB. DOLO 650 mg SOS (if needed) given for fever and pain
Due to medical therapy his symptoms subsided and clearly we can see it in usg reports ( liquefaction) meaning abcess responded to our medical therapy.
4) Is there a way to confirm the definitive diagnosis in this patient?
Ans -
Apart from serological examination which is positive in 94% of the cases..Further confirmation can be done by using Ultrasonography but these are not commonly used
8) Infectious disease
A 50year old male with altered sensorium .
1) What is the evolution of the symptomatology in this
patient in terms of an event timeline and where is the anatomical
localization for the problem and what is the primary etiology of the
patient's problem?
1.
3
years ago- diagnosed with hypertension
2.
21
days ago- received vaccination at local PHC which was followed by fever
associated with chills and rigors, high grade fever, no diurnal variation which
was relieved on medication
3.
18
days ago- complained of similar events and went to the the local hospital, it was
not subsided upon taking medication(antipyretics)
4.
11
days ago - c/o Generalized weakness and facial
puffiness and periorbital oedema. Patient was in a drowsy state
5.
4
days ago-
a.
patient
presented to casualty in altered state with facial puffiness and periorbital oedema
and weakness of right upper limb and lower limb
b.
towards
the evening patient periorbital oedema progressed
c.
serous
discharge from the left eye that was blood tinged
d.
was
diagnosed with diabetes mellitus
6.
patient
was referred to a government general hospital
7.
patient
died 2 days ago
2)
2) What is the efficacy of drugs used along with other non pharmacological
treatment modalities and how would you approach this patient as a
treating physician?
Ans-
Inj.
Liposomal amphotericin B according to creatinine clearance
200mg
Iitraconazole was given as it was the only available drug which was adjusted to
his creatinine clearance
Deoxycholate
was the required drug which was unavailable
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
Ans -
Mucormycosis is may be being triggered by the
use of steroids, a life-saving treatment for severe and critically ill Covid-19
patients. Steroids reduce inflammation in the lungs for Covid-19 and appear to
help stop some of the damage that can happen when the body's immune system goes
into overdrive to fight off coronavirus. But they also reduce immunity and push
up blood sugar levels in both diabetics and non-diabetic Covid-19 patients.







/hyperkalemia-symptoms-5ad4e0b0642dca00363403f9.png)







Comments
Post a Comment