A 40 YEAR OLD MALE WITH ACUTE GASTROENTIRITIS
A 40year old male security guard by occupation from narketpally was brought to casualty by his wife.
CHEIF COMPLAINTS:-
Cold since 3days
Fever since morning
Loose stools since morning
Pain abdomen since morning
HISTORY OF PRESENT ILLNESS -
Patient was apparently asymptomatic 3days ago then he developed cold then he developed high grade fever since morning which is associated with chills and rigors, no aggravating and relieving factors.
-c/o loose stools (10-12episodes) since morning.
-c/o nausea and pain abdomen (umbilical region), diffuse, pricking type of pain.
-No other c/o sob,orthopnea, pnd, chestpain, palpatations.
-No c/o giddiness and lightheadness
PAST HISTORY:
No similar complaints in the past.
No H/o Type II DM , Hypertension, TB, CAD , Epilepsy and Thyroid disorders.
PERSONAL HISTORY:-
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel & bladder: Regular
Patient was a occasionally alcoholic for about 15 years.Usually he consumes beer(1 bottle per one time).
Last intake - 7 days ago
No allergies
DAILY ROUTINE AND LIFESTYLE:
He work as security guard, his routine is active lifestyle
6AM - Wakes up
9AM - Eats breakfast (rice and curry).
Does his duty upto 1pm
2PM - Lunch(rice and curry).
5PM- Tea
Finishes his duty by 7pm and goes to house by 7:30pm
8PM - Dinner(rice and some curry).
FAMILY HISTORY:
No significant family history
GENERAL EXAMINATION:
Patient is conscious, coherent, co-operative to time, place and person and is moderately built and well nourished.
No pallor/icterus/cyanosis/clubbing/Generalized lymphadenopathy/pedal edema.
-Mild Dehydration is present.
VITALS:
Temp: 104°F
PR: 96 bpm
RR: 20cpm
BP: 130/80mmHg
Spo2: 98%@RA
GRBS: 111mg/dl
SYSTEMIC EXAMINATION:
CVS: S1 S2 heard, No murmurs
RS: BAE+
P/A: soft, non tender
No organometally.
CNS examination:
GCS- E4V5M6
Pupils -B/L NSRL
Deep tendon reflexes:
Right. Left
Biceps: +2 +2
Triceps: +1 +1
Supinator:. +1 +1
Knee: +2 +2
Ankle: +1 +1
Plantar: - -
PROVISIONAL DIAGNOSIS -
?ACUTE GASTROENTERITIS.
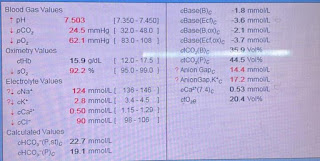
INVESTIGATIONS:-(12/7/2023)
BGT: B-POSITIVE
RBS - 85mg/dl
HEMOGRAM:
Hb: 15.4 gm/dl
TLC: 1100
Platelets :2.30
PBS:NC/NC with WBC leukocytosis
Urea: 18mg/dl
Serum Creatinine: 1.0mg/dl
SERUM ELECTROLYTES:
Na: 136
K:3.4
Cl:99
Ca:1.11
LFT:-
Total bilirubin-2.72
Direct bilirubin-0.50
AST-30
ALT-12
ALP- 159
Total protein-5.8
Albumin-3.67
A/G: 1.72
CUE: Albumin-nil
Sugar- nil
Epithelial cells - 2-4
Pus cells -2-3
Bile pigments-nil
Bile salts-nil
SEROLOGY:
HBsAG - negative
HCV- negative
HIV 1/2 -negative
ECG:-
USG ABDOMEN - No sonlogical abnormalities detected.
TREATMENT -
1)1SACHET ORS IN 1LIT OF WATER 200ML AFTER EACH LOOSE STOOLS EPISODE.
2)INJ.NEOMOL 1GM IV/STAT.
3)I.V FLUIDS 2*NS , 1*RL @100ML/HR.
4)INJ.PAN 40MG IV/BD(AT 8AM AND 8PM).
5)TAB.SPOROLAC DS PO/TID.









Comments
Post a Comment