SHORT CASE - A 45 year old male came to the OPD with the chief complaints of SOB ,tingling sensation and dark stools.
SHORT CASE : FINAL PRACTICAL
MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Viharika Vupputuri
1701006197
June 15,2022.
CASE PRESENTATION
A 45 year old male came to the OPD with chief complaints of
Shortness of breath on exertion since 2 months.
Tingling sensation of limbs since 2 months.
Dark coloured stools since 3 days.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 2 months back then he developed shortness of breath which is insidious in onset grade 2 gradually progressed to grade 3 .
Patient complains of tingling sensation in legs since 2 months .
Patient also complains of dark coloured stools since 3 days.
PAST HISTORY
No similar complaints in the past. Not a known case of hypertension , diabetes , asthma , epilepsy, TB.
Patient had an episode of involuntary movements with drooling of saliva and uprolling of eyeballs 20 years back and was admitted in the hospital and diagnosed as epilepsy and took medication. Later 2-3 episode of seizures were seen within 15 days. Then he had seizure free period.
PERSONAL HISTORY
Diet - Mixed
Appetite - Normal
Bowel and bladder habits - passage of dark coloured stools 3 days back , one episode per day
Addictions - Used to consume alcohol daily since 12 years about 90 ml everyday.
Alcohol abstinence since 2 months
No allergies
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient is conscious, coherent and cooperative and well built and moderately nourished.
Patient is examined in a well lit room.
Pallor - present
No signs of icterus, clubbing, cyanosis, lymphadenopathy and edema.
VITALS-
Temperature- afebrile
BP- 110/80
RR- 16cpm
PR - 80bpm
SYSTEMIC EXAMINATION
CVS
S1 ,S2 heard
No murmurs
RS - NVBS heard
CNS - normal
Per abdomen
Soft , non tender
No organomegaly.
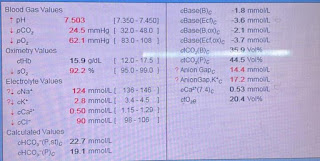
INVESTIGATIONS
10/6/22:
CBP:
Hb : 3.2 g/dl
TLC: 3,400 cells/cumm
Neutrophils: 42
Lymphocytes: 56
Eosinophils: 0
Monocytes: 02
Basophils: 0
PCV : 9.2
MCV: 117.9
MCH: 42
MCHC: 34.8
RDW-CV: 24.2
RBC: 0.78
Platelets: 68,000
ESR: 40
Reticulocyte count: 0.5
LFT:
TB: 2.69
DB: 0.70
ALT: 14
AST:51
ALP: 115
TP: 5.8
Albumin: 3.6
A/G: 1.69
RFT:
Blood urea: 16
Serum Creatinine: 0.8
Serum Uric acid: 7.8
Serum Electrolytes:
Serum Calcium: 8.9
Serum Phosphorus: 3.9
Na+: 133
Cl: 107
K+: 3.8
RBS: 104
LIPID PROFILE:
Total cholesterol: 90
Triglycerides: 116
HDL: 24
LDL: 49
VLDL: 23
12/6/22:
Hb: 2.8 g%
TLC: 2380
Neutrophils : 36
Lymphocytes: 60
Eosinophils:0
Monocytes: 4
Basophils: 0
PCV: 8
MCV: 115.8
MCH: 39.8
MCHC: 34.3
RDW-CV: 33.5
RBC: 0.69
PLT- 72,000
Peripheral smear - Anisopoikilocytosis with hypochromia with microcytes, macrocytes and pencil cells.
CLINICAL IMAGES
PROVISIONAL DIAGNOSIS
Pancytopenia 2°to vitamin B12 deficiency.
TREATMENT
INJ. VITCOFOL 1000mcg/IM/OD × 7 days
INJ. OPTINEURON 1AMP in 100ml
TAB. PANTOP 40mg/PO/OD





Comments
Post a Comment