INTERNSHIP LEARNING ASSESSMENT
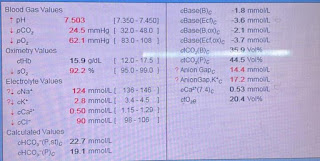
INTERNSHIP LEARNING EXPERIANCE PAJRs I created around 3 PAJR groups and updated critical data about the patient like his ECG, Chestxray, 2D-Echo, Feverchart. PAJR mainly consists of blogs and soapnotes SOAP NOTES Soap notes consist of complaints, Vitals, Diagnosis and Treatment of patient. FEVER CHART In medicine department my pgs taught me how to plot fever chart,importance of fever chart . PERIPHERALS I learnt - To d raw samples from radial and femoral artery. - Took ABG sample - Performed CPR - Secured multiple cannula - Inserted Foley’s catheters, condom catheter and Ryle’s tube - Monitored vitals of all patients either hourly. -Attended rounds for ICU and AMC cases. NEPHROLOGY AND WARD DUTY - Assisted how to secure a central line - Give IV injections - Seen the complications of dialysis - Monitored the patients undergoing dialysis - Observed multiple CKD cases requiring dialysis. PSYCHIATRY - I learnt alot of cases about Schizophrenia, dep...